Addictions
“Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry … Addiction is characterized by inability to consistently abstain, impairment in behavioral control, craving, diminished recognition of significant problems with one’s behaviors and interpersonal relationships, and a dysfunctional emotional response. Like other chronic diseases, addiction often involves cycles of relapse and remission. Without treatment or engagement in recovery activities, addiction is progressive and can result in disability or premature death.”—American Society of Addiction Medicine
(This is a short definition of addiction that appears at the beginning of an 8-page-long definition adopted by ASAM; https://www.asam.org/resources/definition-of-addiction.)
As exemplified in the above statement by ASAM, today most professionals in the fields of medicine, mental health, and addiction treatment accept the disease model of addiction. See Addiction and the Brain section for additional information.
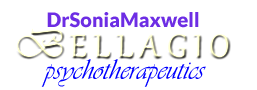
Source: SAMHSA, 2019, Fig. 1
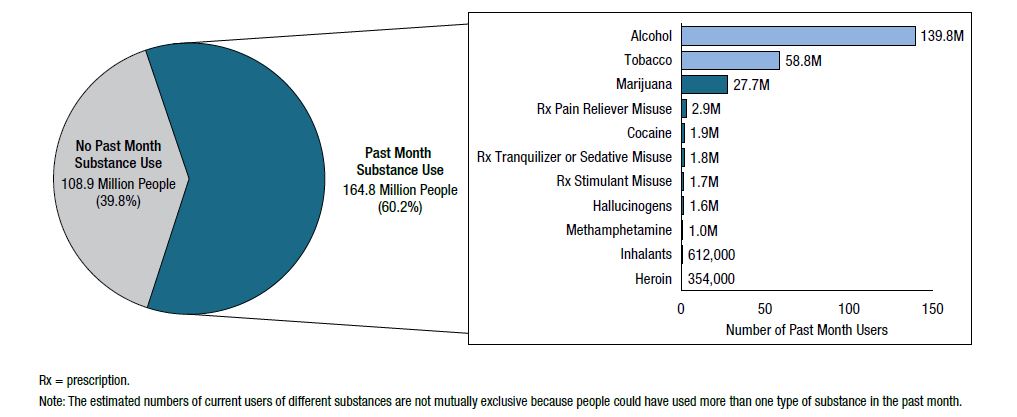
Source: SAMHSA, 2019, Fig. 10
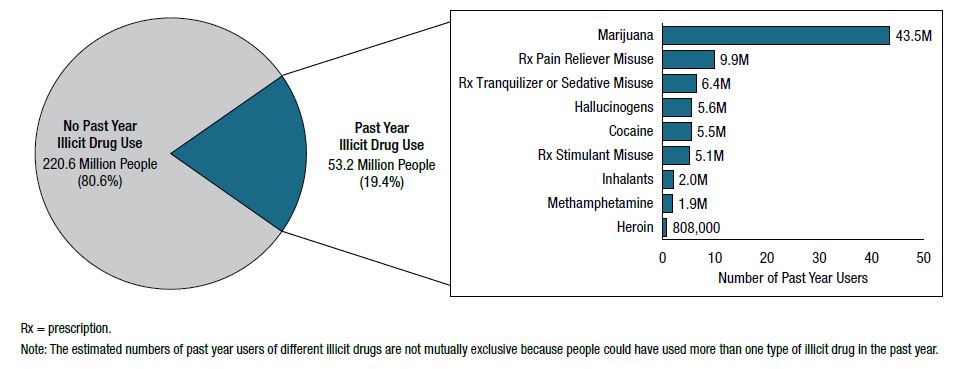
Source: SAMHSA, 2019, Fig. 42
In my practice, I treat the context of addiction as well as the mental health side of a dual diagnosis (aka co-occurring disorders). In the latter case, a client typically comes to see me in the aftercare phase or as someone whose symptomatology falls under Category I of the Quadrants of Care Model developed by the National Association of State Alcohol and Drug Abuse Directors and the National Association of State Mental Health Program Directors (see the Dual Diagnosis section).
Context refers to issues such as poor self-concept (self-esteem, self-worth, self-efficacy), adverse childhood experiences and other family of origin problems, intimate relationship dysfunction, and work challenges. This does not mean that the client has a mental health diagnosis in addition to addiction; it simply may be the case of suboptimal functioning in one or more areas. Addressing these areas helps the client in his/her recovery process.
Dual diagnosis refers to meeting the criteria for addiction as well as for one or more other mental health disorders. Approximately 50% of people with addiction will experience another mental health disorder and vice versa.
While the term addiction is commonly used by both professionals and the public, the official language is slightly different. The above definition of addiction corresponds most closely with the diagnosis of severe substance use disorder (e.g., Alcohol Use Disorder, Severe, code F10.20) as defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-5, published in 2013 by the American Psychiatric Association). The severity of a substance use disorder is based on the number of symptoms the individual experiences. As a general estimate, mild refers to 2-3 symptoms, moderate to 4-5, and severe to six or more symptoms out of 10-11 that are listed as diagnostic criteria.
Substance use disorders encompass 8 separate classes of drugs: alcohol, cannabis, hallucinogens, inhalants, opioids, sedatives/hypnotics/anxiolytics, stimulants (including cocaine and amphetamine-type substances), and tobacco.

Source: DavidSusman.com
Common Features of Substance Use Disorder
There is a common cluster of cognitive, behavioral, and physiological symptoms, as well as underlying changes in brain circuits that may persist. The following 11 diagnostic criteria exist across all 8 classes of drugs (exception: the criterion of withdrawal is not listed in the DSM-5 for hallucinogens and inhalants):
Impaired control over substance use
1. Taking larger amounts or over a longer period than was originally intended
2. Trying to reduce or stop the use of the substance, with multiple unsuccessful efforts to do so
3. Spending a great deal of time obtaining, using, or recovering from the substance (in severe cases, virtually all of the daily activities revolve around this)
4. Experiencing craving, that is, an intense desire or urge for the substance (reward structures in the brain are activated, making it difficult to think of anything else), which often signals an impending relapse
Social impairment due to substance use
5. Failing to fulfill major role obligations at work, home, school, or community
6. Giving up/reducing important activities, including recreational activities previously enjoyed
7. Withdrawing from family, missing activities, refusing to talk to loved ones
Risky use of the substance
8. Using the substance in hazardous circumstances, such as driving, swimming, or operating machinery
9. Failing to abstain from using the substance despite the difficulty it is causing
Pharmacological criteria
10. Tolerance: An increased dose is needed to achieve the desired effect, or the effect is reduced when the usual dose is consumed. Changes are seen in how the substance affects the central nervous system, such as how it has previously affected respiratory depression, feelings of sedation, and motor coordination
11. Withdrawal: Behavioral, cognitive, and physiological changes that occur when someone who has engaged in heavy, prolonged substance use suddenly stops or significantly reduces such use
NOTE: Although tolerance and withdrawal are common features, neither is required for the diagnosis of a substance use disorder.
How Substance Use Begins
In general, the initial decision to try alcohol or other drugs is voluntary. If the first use produces positive effects, the individual may turn to the substance again in order to feel the desired effect. Here are some common reasons why people start to use drugs:
- Curiosity and social pressure—As you may have guessed, this is particularly true of teens. Adolescence is a time marked by significant changes in the socioemotional context as teens increasingly meet their social needs (including acceptance, friendship, and emotional support) away from their families. Acceptance into peer groups becomes crucial, and with it the need to meet peer standards, whatever they may be
- To do better—Examples are the desire to improve focus, performance, or endurance in school, at work, or in sports
- To numb negative feelings—This is often associated with anxiety (including in social situations), trauma, stress, depression, and problems with self-esteem
- To feel good—It is common knowledge that the initial effect of a drug is often an intense feeling of pleasure or euphoria. With illicit stimulants, such as cocaine, the high is typically followed by feelings of power, self-confidence, and increased energy. Opioids, such as heroin, produce feelings of relaxation and general well-being after the initial high
 How Substance Disorders Begin
How Substance Disorders Begin
- Before addiction sets in, it is possible to stop substance use without a great number of adverse consequences
- At some indeterminate point in time, the ability to walk away from substance use is lost and the individual has become addicted because the brain has been changed
- From this point forward, substance use becomes an overwhelming compulsion and free choice no longer exists
Go to the section on Addiction and the Brain to learn more.
Risk Factors
The most prominent risk factors are biology, environment, and the route of administration.
Biological Factors
- Genetic makeup (e.g., inherited predisposition to abuse alcohol because of father’s alcoholism)—Research suggests that genetic factors account for between 40 and 60 percent of a person’s susceptibility to addiction. Multiple genes may be responsible for transmitting addiction vulnerability from one generation to another, which is known as “polygenic inheritance.” The genetic component of addiction can skip generations or affect some members of a family and not others, based on the combination of genes an individual inherits
- Gender (e.g., rates of alcoholism are almost three times as high among adult men than adult women)
- Mental health—Individuals with other (non-SUD) mental health disorders are at greater risk of drug use and addiction
- Age—Early use is a strong predictor of serious problems, including addiction, in part due to the high likelihood that the substance(s) will have a harmful effect on the developing brain
Environmental Factors
- Home and family—Various adverse childhood experiences such as a chaotic home, neglect, substance use by parent or caregiver, older family members who use substances but are seen as role models
- Peers, school, and work—Peer influence (for teens especially, but also for adults), poor social skills, poor school or work performance
- Community—Even if family environment does not present a risk, community attitudes toward drugs may prevail
Route of Administration
- When a drug is smoked or injected, it enters the brain within seconds
- The pleasure or euphoria is extremely high but typically fades within minutes
- The drug’s addictive potential is increased because individuals resort to more frequent drug taking in an attempt to recapture the extreme pleasurable state
Treatment of Addiction
- Yes, addiction is a treatable disorder, with many options
- No, addiction is typically not “cured” because it is a chronic disease, just like hypertension or asthma (see the graphic below for a comparison)
- Yes, addiction can be managed successfully by committing to lifelong recovery
- No, relapse does not mean that there is a permanent failure of addiction treatment
- In spite of the challenges brought on by addiction, research has shown that the brain has a remarkable capacity to recover, either fully or partially, after a prolonged and sustained abstinence from drug abuse
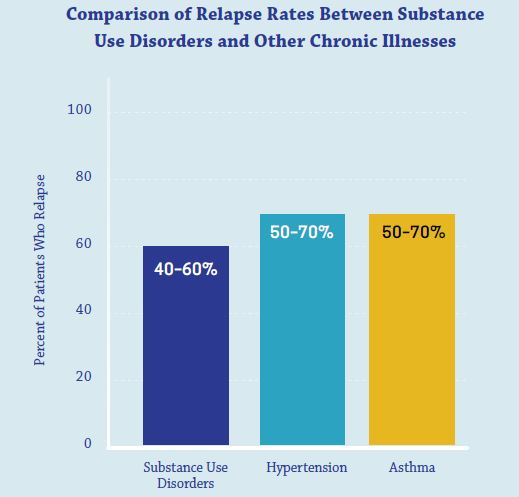
Source: National Institute on Drug Abuse, 2018
A Final Note About the DSM-5
Substance-related disorders are grouped together with addictive disorders in the DSM-5 because they activate the brain reward system in similar ways. Currently, the section on addictive disorders contains just the Gambling Disorder, with additional disorders possibly on the way in the next update or sooner. Other so-called “behavioral addictions,” such as those related to compulsive sex, exercise, shopping, or Internet gaming are not officially recognized in the DSM-5 because there is insufficient evidence to identify them as mental disorders.
Content based in part on the following public domain sources:
• American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013
• National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction (NIH Publication No. 18-DA-5605). U.S. Department of Health and Human Services, 2018
• Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068). SAMHSA, 2019