Dual Diagnosis
The term dual diagnosis (also known as co-occurring disorders or COD) indicates that an individual’s symptoms meet the criteria for one or more substance use disorders (SUD) as well as for one or more non-SUD mental health disorders. Because these disorders co-occur, their symptoms interact to create a complex and unique problem that can worsen the course and outcome of both.
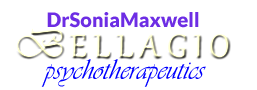
According to a recent national survey, 19.3 million adults in the U.S. have a substance use disorder. Of those, about 48% also suffer from a mental health problem, which means that 9.2 million adults meet the diagnostic criteria for both an SUD and a non-SUD mental health disorder.
Source: SAMHSA, 2019, Fig. 53
The severity associated with having both is heightened because the interaction of two conditions produces a synergistic effect, which results in an overall condition that is harder to treat. Furthermore, the interaction takes place not just physiologically but also psychologically. Just as untreated SUD is likely to render mental health treatment ineffective, untreated mental health issues make sobriety difficult to achieve and maintain.
Many combinations of dual diagnosis exist. When the population prevalence of mental health disorders and the commonality of co-occurrence are taken into account, the most common combinations are with trauma-related disorders (e.g., PTSD), anxiety and mood disorders, and ADHD.
Either disorder can develop first (SUD or non-SUD). This does not necessarily mean that the first disorder to appear caused the other.
Researchers have attempted to explain why the dual diagnosis is a common condition:
- Common risk factors—A number of genes have been found to contribute to the risk of developing both a substance use disorder and a mental health disorder. For example, some people have a specific gene that puts them at increased risk of a mental health disorder in adulthood if they were frequent users of cannabis as minors. A gene can also influence the intensity with which someone responds to a drug. In addition, environmental factors, such as stress or trauma, can cause genetic changes that are passed down through generations and may contribute to the development of mental health or substance use disorders
- Mental health problems as contributing factors—Some mental health conditions have been identified as risk factors for developing an SUD, including unipolar and bipolar depression; anxiety and trauma-related disorders (e.g., Social Anxiety Disorder, PTSD); ADHD; psychotic disorders (e.g., Schizophrenia, Schizoaffective Disorder); Oppositional Defiant, Conduct, and Intermittent Explosive Disorders; and Borderline and Antisocial Personality Disorders. An individual with a mental health disorder may have brain changes that enhance the rewarding effects of the substance, thus predisposing the person to become addicted. Sometimes, the initial motivation behind using an SUD is self-medication, such as:
- An individual experiencing PTSD turns to alcohol or other drugs to cope with overwhelming symptoms
- Someone with Social Anxiety Disorder starts using drugs to feel less anxious and inhibited (according to research, there is a strong association between this disorder and cannabis use)
- A person with ADHD (in particular an adult whose ADHD has never been diagnosed) uses stimulants to help with concentration
- Substance use and addiction as contributing factors—Substance use may change the brain architecture in ways that make a person more vulnerable to a mental health problem
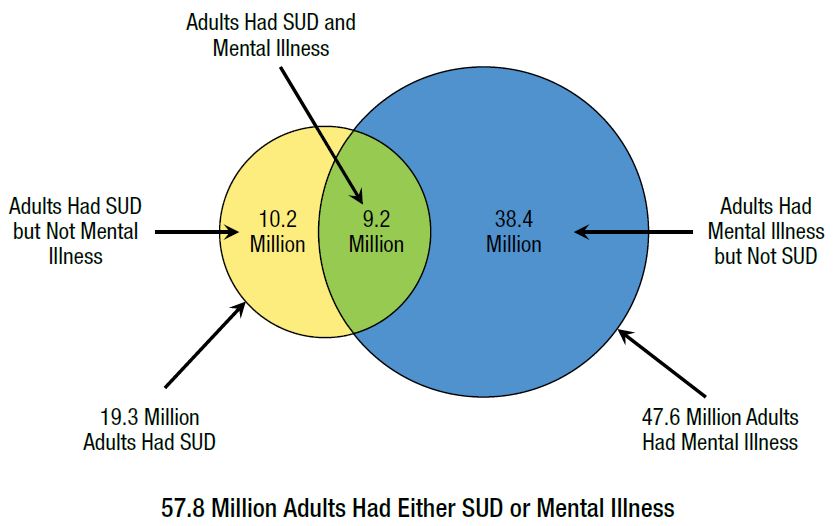
According to the 2018 national survey referenced above, of the 9.2 million adults with co-occurring disorders, only 7.0% received the recommended combination of mental health treatment and a specialty substance use treatment. That figure is similar to the results of prior national surveys dated 2015-2017.
Source: Adapted from SAMHSA, 2019, p. 64
For someone entering SUD treatment while also suffering from one or more co-occurring mental disorders, it is crucial to choose a place that offers the option of concurrent, integrated treatment for all conditions. Untreated mental health conditions are one of the main reasons for repeated relapse among individuals with SUD. Substance Abuse and Mental Health Services Administration (SAMHSA) guidelines, as well as those of American Society of Addiction Medicine (ASAM) and many other professional associations, recommend integrated treatment that coordinates substance abuse and mental health interventions to treat the whole person more effectively.
When considering treatment for dual diagnosis, it helps to conceptualize the problem based on the severity of each. Someone with mild anxiety and mild SUD is not going to need the same type of treatment as a person who has suffered from severe SUD and anxiety for several years. The Quadrants of Care Model illustrates this very well. Developed by the National Association of State Alcohol and Drug Abuse Directors (NASADAD) and the National Association of State Mental Health Program Directors (NASMHPD), the model is a classification of recommended services based on the severity of each COD component.
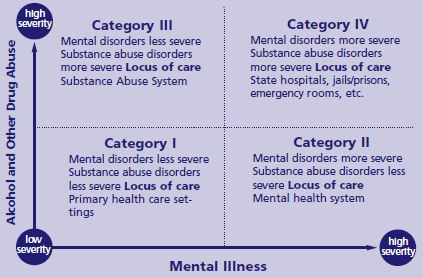
Source: SAMHSA, 2019, p. 51
The image above is the original model, which has since been modified by the National Council for Community Behavioral Healthcare. The modified model accommodates individual choice of treatment, while at the same time directing primary care and specialty mental health and substance use disorder systems to create specific protocols for high-risk individuals (e.g., those with severe mental issues and severe SUD who choose to seek services in a Category I setting of primary health care, which is not recommended in the original model). The original model makes more sense for my work as a private practice clinician. To see the modified model, go to this link https://www.integration.samhsa.gov/resource/four-quadrant-model
To keep reading about integrated COD treatment and addiction treatment in general, click here.
Content based in part on the following public domain sources:
• American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013
• Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068). SAMHSA, 2019
• Substance Abuse and Mental Health Services Administration. Substance Abuse Treatment for Persons With Co-Occurring Disorders, TIP 42 (HHS Publication No. 13-3992). SAMHSA, 2013